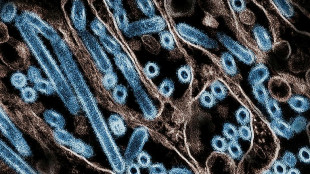
Second US monkeypox death as virus linked to brain inflammation
A second US death was linked to monkeypox on Tuesday as health authorities published a study describing how two previously healthy young men experienced inflammation of the brain and spinal cord as a result of the virus.
There have been nearly 22,000 US cases in the current global outbreak, which began in May, but new infections have been falling since mid-August as authorities have distributed hundreds of thousands of vaccine doses.
The latest fatal case involved a severely immunocompromised resident of Los Angeles County who had been hospitalized, the local health department said, without revealing further details about the case.
"Persons severely immunocompromised who suspect they have monkeypox are encouraged to seek medical care and treatment early and remain under the care of a provider during their illness," the department said.
The first US death linked to the viral illness occurred in Texas and was announced on August 30, although authorities said that as the person was severely immunocompromised, they were investigating what role monkeypox had played.
The current global outbreak is primarily affecting men who have sex with men.
Historically, the virus has been spread via direct contact with lesions, body fluids and respiratory droplets, and sometimes through indirect contamination via surfaces such as shared bedding.
But in this outbreak, there is preliminary evidence that sexual transmission may also play a role.
- Brain and spinal cord inflammation -
The US Centers for Disease Control and Prevention meanwhile published a report about two unvaccinated men in their 30s who experienced brain and spinal cord inflammation after testing positive for the virus.
The first, patient A, was a gay man in his 30s from Colorado whose symptoms began with fever chills and malaise but progressed to rashes on his face, scrotum and extremities, with swabs of lesions testing positive for the virus.
He also developed lower extremity weakness and numbness, was unable to empty his bladder, experienced a persistent and painful erection, and was hospitalized.
Magnetic resonance imaging (MRI) revealed brain and spinal cord inflammation, and he was treated with the oral monkeypox antiviral tecovirimat as well as other drugs, and began to improve at two weeks.
He was released but continued to have left leg weakness and required an assistive walking device at one month followup.
A second person, patient B, was also a gay man in his 30s from the capital Washington. His fever, rashes and muscle pain progressed to bowel and bladder incontinence and progressive flaccid weakness of both legs.
Brain and spinal cord inflammation was confirmed on MRI and he was intubated in an intensive care unit, where he was treated with intravenous tecovirimat, as well a drug to reduce inflammation, and finally blood plasma exchange.
He remains in hospital but can walk with the assistance of a device.
The report said the underlying mechanism behind the two cases was unclear -- it might have been direct invasion of the central nervous system, or an autoimmune response triggered by monkeypox infection elsewhere in the body.
E.Fisher--MC-UK